WVSOM recognized as nationwide leader ‘in producing graduates who practice in rural settings’
WV Staff Report
LEWISBURG, W.Va. – “It’s that balance. While we’re a leader in rural primary care, and, first and foremost, we’re serving West Virginia and populating the state with our grads, you can also come to WVSOM and be those other types of physicians that people want to be – dermatologists, ophthalmologists, orthopedic surgeons, you name it.”
West Virginia School of Osteopathic Medicine President James Nemitz explained the school’s medical opportunities this week.
While Nemitz has served as WVSOM’s seventh president since 2018, he has been a steady presence at the school for well over three decades.
Since its founding more than a half-century ago, WVSOM has established itself as a nationwide leader “in producing graduates who practice in rural settings.”
According to a recent article from U.S. News and World Report, WVSOM ranks 26th in the nation for “graduates practicing in medically underserved areas,” and 19th for “graduates practicing in rural areas.”
This fact is made considerably more impressive when factoring in the cost of education, as WVSOM offers some of the lowest medical-school tuition rates in the United States.
While Nemitz has served as WVSOM’s seventh president since 2018, he has been a steady presence at the school for well over three decades.
“Many of the challenges concern training new physicians in the environment they’re going to work in,” Nemitz said, in explanation of what makes WVSOM stand apart from other medical schools. “A lot of residency programs are in urban areas, and being trained in an urban area doesn’t necessarily prepare you for rural practice.”
“What WVSOM has been so successful at is exposing our students to a rural environment throughout their experience,” Nemitz continued. “The first two years, they’re here in this small town of Lewisburg. But in their third and fourth years they are distributed around the state to other rural areas.”
“Our students learn an appreciation for rural practice, and they get to see how it’s done,” Nemitz added.
According to Nemitz, community-based residency programs – known as “teaching health centers” – have become a vital partner in the education of rural physicians. These teaching health centers are federally funded through HRSA (Health Resources and Services Administration).
“We’ve been working with two of them – Access Health in the Beckley-area, and Cornerstone (Health), which is across the border in Pennsylvania,” Nemitz noted. “These are residencies where the person is training in a more rural environment, but they still get hospital training through an affiliated hospital.”
Nemitz further explained that, due to both convenience and geography, residents often receive their training in “big hospitals,” adding that most residents in West Virginia are trained at CAMC (Charleston Area Medical Center), WVU Medicine, or through the Marshall University system.
“It’s these smaller, community-based residencies that really have a niche,” Nemitz said. “One of the challenges with getting physicians into rural areas is the training – training the person to deal with the issues that they’ll face in rural areas.”
Those issues, according to Nemitz, center around the isolated nature of a rural environment. Resources are often in shorter supply, and frequently farther away, while assistance is not always on the other end of a phone call.
“These are real issues that you see in West Virginia that impact care,” Nemitz added. “The rural physician may be the only person in their area. I met one of our alums recently, now this was in rural Georgia, but he was the only physician in five counties. That’s part of the challenge.”
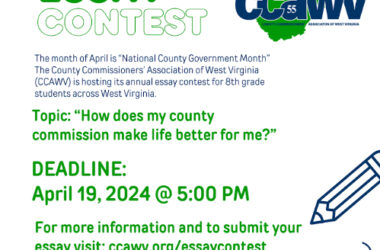
“At WVSOM, we’re proud of the fact that we’ve populated pretty much all of West Virginia with our graduates,” Nemitz said, adding that WVSOM graduates are currently practicing medicine in 51 of the state’s 55 counties.
Nemitz believes that it is the lack of medical facilities in West Virginia which prevents WVSOM graduates from practicing in all 55 counties, noting that, “The biggest challenge is access to care.”
“Quite frankly, the biggest issue is getting people to the provider,” Nemitz said. “Transportation is a huge issue – actually getting people to the doctor, or to the clinic, or to the rural hospital.”
Another obstacle to the recruitment of rural physicians are lifestyle-concerns. According to Nemitz, everything from recreational activities, to the social landscape, to salary considerations weigh heavily upon an individual’s decision as to where they wish to practice medicine.
“Everybody envisions a certain lifestyle for themselves,” Nemitz said. “Does that rural area have the things that a person is looking for?”
While a primary goal of WVSOM is “to produce the best educated, most caring and compassionate osteopathic physicians in the world,” a core principle of the school’s mission statement is it’s unwavering dedication to “the State of West Virginia and the health care needs of its residents, emphasizing primary care in rural areas.”
As of the start of 2023’s fall semester, WVSOM is fully accredited by both the American Osteopathic Association (AOA), and the Higher Learning Commission (HLC). Recently, full tuition waivers have been made available for qualifying West Virginia resident-students. Non-resident students may also have the option of utilizing a tuition-waiver program should they decide to remain in West Virginia to practice after graduating. A full listing of scholarships and financial aid programs are available on the school’s website, at wvsom.edu.
“Education is our primary purpose,” Nemitz said. “Our job is to prepare our students to be the best physician – the best osteopathic physician – that they can be, and be able to go into whatever specialty they choose.”
“The reality is that we need all kinds of physicians,” Nemitz added. “It’s not just primary care physicians. We need surgeons, we need cardiologists, we need nephrologists – all of those other types of specialties are needed, and we produce those as well. ”
“You can come to WVSOM and be whatever type of physician you want to be, you’re not limited by coming to our school,” Nemitz concluded.